Portable Health Clinic for Digital Health: Current Practices and Opportunities
Rafiqul Islam Marufa , Ashir Ahmed b , Kimiyo Kikuchi c , Fumihiko Yokota d , Helen Benedict Lasimbang e , Lutfan Lazuardi f , Faiz Shah g , and Naoki Nakashimaa
aMedical Information Center, Kyushu University Hospital, Japan
bDepartment of Advanced Information Technology, Kyushu University, Japan
cDepartment of Health Science, Kyushu University, Japan
dInstitute for Asian and Oceanian Studies, Kyushu University, Japan
eHospital of University Malaysia Sabah, University Malaysia Sabah, Malaysia
fFaculty of Medicine, Public Health and Nursing, Gadjah Mada University, Indonesia
gYunus Center, Asian Institution of Technology, Thailand
Abstract
The concept of the Portable Health Clinic has been established to overcome the limitations of the commonly practiced digital healthcare systems. The absence of infrastructure and shortage of medical human resources are the two major obstacles to ensuring quality healthcare services to the unreached rural communities. The PHC is an affordable, sustainable and usable digital healthcare system for such unreached communities. This system uses a smart application in a combination of various medical sensors in a very efficient way and the community health workers provide home delivery service with the support of a remote doctor. Although the PHC system was initially designed and developed for primary care, gradually this modular system added new modules for non-communicable diseases, pathology, eye care, maternal & child health, and COVID-19. Currently, the PHC team is working on the expansion in the areas of communicable disease, mental health, and post-disaster care. This session has been designed to present the current practices of this system in different countries and to discuss the future opportunities of this potential system to cover other areas in need.Keywords
Digital health, tele-pathology, tele-eyecare, maternal and child health care, mental health, communicable and non-communicable diseases, disasterIntroduction
Digital Healthcare is very common practice with the development of new cuttingedge technologies [1-2]. The growing wide-scale Internet coverage all over the world makes it easy to reach digital healthcare services to the far end [3-4]. However, there are still a lot of challenges to getting the benefit of this new system in the unreached communities of the developing countries [5]. The Portable health Clinic system has been developed as a vehicle to overcome these challenges.Portable Health Clinic
Portable Health Clinic (PHC) is an affordable, sustainable, and simply useable digital healthcare system for the rural communities of developing countries [6-9]. However, it can also be convenient for providing better care to the aging communities through home delivery services in the developed world [10-11]. Thus, it can be a very effective tool for reaching quality healthcare services to the unreached communities to ensure Universal Health Coverage (UHC). As PHC is a modular system, it can expand its services as per demand. Starting with primary care with the focus on non-communicable diseases (NCDs), it has already added a tele-pathology module, a tele-eye care module, a maternal and child health care module and a COVID-19 module.Basic Model of the Portable Health Clinic
The basic model of the PHC system was developed for primary care with a special focus on NCDs as the main cause of death in Bangladesh [12]. This PHC system has four basic components. These are 1) PHC box with basic medical sensors for measuring a patient’s BMI, hipwaist ratio, pulse rate, body temperature, blood pressure, blood glucose, hemoglobin, uric acid, urine protein, urine sugar and arrhythmia, 2) PHC online software system, 3) community health workers and 4) city call-center doctors.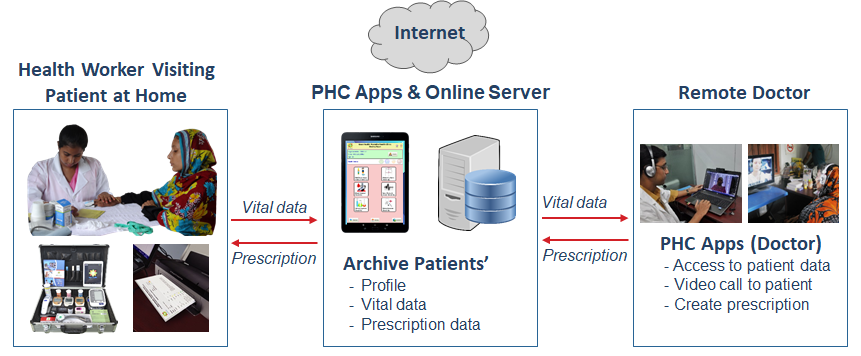 Figure 1: PHC System Diagram
Figure 1: PHC System DiagramThe community health worker visits a patient at home as per schedule or on-demand. The health worker brings with the PHC box to measure the vital information and upload this data with the medical history of the patient to the online server using the system apps. The remote doctor gets access to this data and makes a video call to the patient for further verification. Finally, the doctor produces an online prescription and passes it to the patient through the health worker [Figure 1]. The whole process to serve one patient takes about 15 minutes excluding the doctor`s consultancy time.
Tele-Pathology Module
The PHC system added this tele-pathology module to produce additional reports as per the demand of the consulting doctor for better diagnosis [12-13]. The tele-pathology module enables the rural diagnostic centers operated by laboratory technologists (diploma certified) for producing a quality pathological report with the support of the qualified remote pathologist [Figure 2]. At present, this system is capable of blood hematological (CBC) tests, routine examination of urine, routine examination of stool, and skin scarping tests. In this system, the rural laboratory technologist (1) collects the sample, prepare the physical report, produce a test slide, (2) take a number of microscopic images of the slide with varying position, and then (3) upload the images together with the physical report to the online server. The remote pathologist then (4) diagnoses the sample based on the microscopic slide images with the reference of the physical report, finalizes the pathology report, and preserves it on the online server.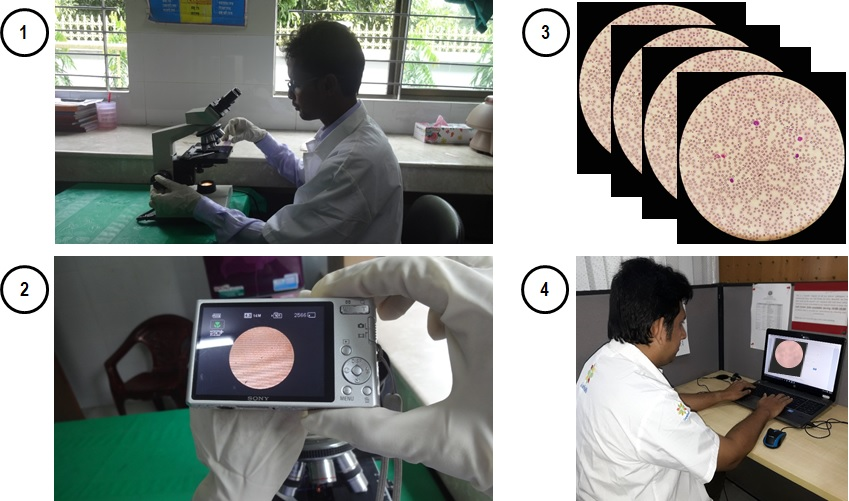 Figure 2: Tele-Pathology System Diagram
Figure 2: Tele-Pathology System Diagram
Tele-EyeCare Module
The Tele-EyeCare module of the PHC system ensures primary eye care services for rural communities [12]. This module has added a Digital Fundus Camera to the PHC box for retinal imaging (both Mydriatic & Non-Mydriatic) of the patients. This enables the health workers to have a better view of the retina and the peripheral for identifying the problem with certainty. Thus, the trained local health workers check and classify the patients as per the severity of the problem. Low-risk patients with simple complications are served by the health workers. However, in case of doubtful cases, the patients` vital information, initial primary checkup reports, and ophthalmic images are shared with a remote ophthalmologist using the online server [Figure 3]. Figure 3: Tele-Eye Care System Diagram
Figure 3: Tele-Eye Care System Diagram
The ophthalmologist then checks the initial primary checkup reports, investigates the ophthalmic images, and provides online prescriptions. If needed, the ophthalmologist can talk to the patient over video call or ask for further investigation. Thus, this system enables the health workers to provide basic eye care service to ordinary patients and special care to the critical patients by the professional ophthalmologist who really deserves special attention.
Tele-MCH Care Module
There is a huge need for MCH services in the rural communities of developing countries. As there is no specialized MCH service in the local medical facilities, in most cases, village women depend on local midwives who mostly do not have any professional training. Therefore, PHC staffs receive a huge number of requests for this specialized service and thus, this MCH care module has been developed [14].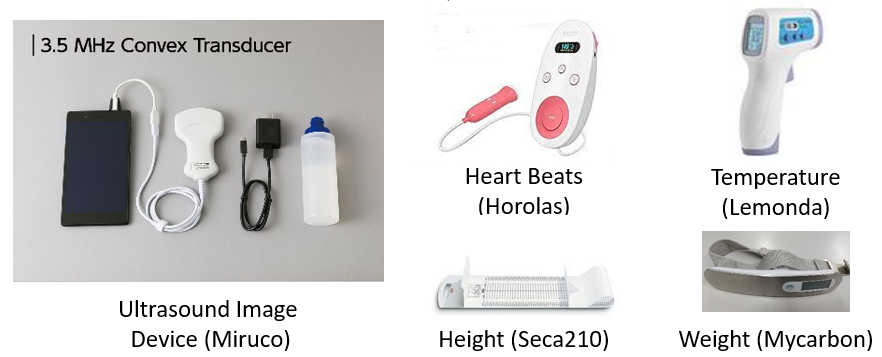 Figure 4: Additional Devices in the MCH System
Figure 4: Additional Devices in the MCH System
The MCH care module basically follows the 8-stages continuum care policy promoted by the WHO for antenatal and postnatal care. In addition, it has added two more care for both the mother and the child at the age of 6 months and 1 year of the baby. The MCH service box includes a few additional pieces of equipment with the basic equipment of the PHC system. These are handheld ultrasound, fetal Doppler, infant height measure meter, infant scale, and pediatric stethoscope [Figure 4]. Since the MHC care service of the PHC system is delivered at home, it ensures a higher participation rate in attending continuum care.
PHC COVID-19 Module
The sudden appearance of the COVID-19 pandemic created a huge panic all over the world as there was no preparation to tackle this highly infectious disease. The good thing with the COVID-19 positive cases is that about 80% of patients are in a less vulnerable group and they can be treated at their homes in a quarantined state. Considering the support to this large group of patients, the PHC for the COVID-19 system has been developed [15]. Using its tele-healthcare facilities, this system can monitor the patients’ health status, follow-up, and provide doctor`s consultancy from distance [Figure 5]. This telehealth system ensures the safety of the health workers and doctors as they serve the patients from distance. The patients also feel safe being isolated from other patients. Besides, the monitoring, follow-up, and treatment of the patients, this system introduces a questionnaire-based triage function considering the Japanese triage system as a basis for early detection of the suspected COVID-19 patients. Figure 5: PHC COVID-19 System
Figure 5: PHC COVID-19 System
This triage system does not confirm COVID-19 positive case but identifies highly suspected subjects who need confirmation RT-PCR test. This could contribute to preventing unwanted crowds at the test centers with limited testing facilities and making the best use of the valued resources.
Upcoming Modules and New Developments of the PHC System
Currently, the PHC team is working on the expansion of its services in the areas of communicable disease, mental health, dental care, and post-disaster care [16-18]. Besides, there are some running studies on the standardization of the PHC data and data visualizations [19-20]. This PHC research and development activities and its implementations are now being done in different Asian countries including Bangladesh, India, Indonesia, Japan, Malaysia, Pakistan and Thailand. Soon these activities will be extended to China, Kenya and Nepal.Panel Discussion
This panel discussion session has been designed to present the current practices of this system in different countries through our partners, their ongoing researches and to discuss the future opportunities of this potential system to cover other areas in need. The global researchers’ team will also focus on the challenges and the possible solutions from their invaluable real field experiences.
Panelists:
Dr. Rafiqul Islam Maruf
Dr. Islam is working as an Associate Professor at Medical Information Center of Kyushu University Hospital under Kyushu University, Japan. Besides, he has been working as a Director of Global Communication Center, the ICT based R&D wing of Grameen Communications, Bangladesh. Earlier Dr. Islam worked in Japanese IT industries for 12 years after completing his Ph.D. in Information Engineering from Hokkaido University, Japan. Throughout his career, he has been involved in research and development of various ICT based social services in various fields including agriculture, education, environment, healthcare and telecommunication. His current research areas include global healthcare, telemedicine, digital health and healthcare services for unreached communities.
Dr. Ashir Ahmed
Dr. Ashir is an Associate Professor at the Faculty of Information Science and Electrical Engineering of Kyushu University. His research aims to develop disruptive technologies in the areas of healthcare and mobility for unreached communities. Digital Healthcare, Healthcare Data Science, Social Business Entrepreneurship, ICT4D are his major research areas. Prior to Kyushu University, he worked at Avaya Labs and NTT Communications to develop VoIP applications and their standardizations. He received his PhD in Information Science from Tohoku University, Japan.
Dr. Kimiyo Kikuchi
Dr. Kikuchi is a lecturer at the Faculty of Medical Science, Kyushu University, and a principal investigator of the Portable Health Clinic for Newborn, Maternal and Child research project. She specializes in Global Health, and her primary research interests are Maternal and Child Health and Telehealthcare. In addition, she contributed as the primary researcher of Ensure Mothers and Babies Regular Access to Care (EMBRACE) project to ensure the continuum of care in maternal and child health, which embodies the "New International Health Policy 2011-2015" of the Japanese government, announced at the MDGs UN Summit.
Dr. Fumihiko Yokota
Dr. Yokota is an Associate Professor at the Institutes for Asian and Oceanian Studies at Kyushu University. He received a Master of Public Health at University of California, Los Angeles in 2001 and Ph.D. in Public Health & Tropical Medicine at Tulane University in the US in 2007. He has more than 15 years of epidemiological research experience in over 10 countries including Indonesia, India, Bangladesh, Thailand, China, Malaysia, Papua New Guinea, and the United States. His current research interests are “Telemedicine for most vulnerable population”, “Aging and mental health in Asia”, “Socio-behavioral epidemiology” and “Methodology and evaluation for transdisciplinary research”.
Professor Helen Benedict Lasimbang
Professor Dr. Lasimbang is the Director of Hospital Universiti Malaysia Sabah (2018-) and also a senior Consultant Obstetrician & Gynaecologist. She practiced as a clinician with the Ministry of Health of Malaysia for 12 years, then in a private hospital for 9 years before joining University Malaysia Sabah in 2012. She is an active member of Professional Medical societies and non-governmental organizations. Her field of interest are women, rural and neglected community health and wellbeing, and reducing alcohol-related harm. Professor Lasimbang published and edited articles in peer-reviewed medical journals and actively organizing community work through Association for Prevention of Alcohol Misuse (APAM) and other organizations.
Dr. Lutfan Lazuardi
Dr. Lazuardi is the head of the Department of Health Policy and Management at the Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, Indonesia. He has been worked in digital health projects at regional and national level in Indonesia, including telemedicine, electronic health record, cancer and disease registry as well as biobanking information system. Recently, he set up and lead the Digital Health Innovation Studio with the aim to facilitate the transformation of innovative ideas into marketable product. Some of the products has been used in many health facilities in Indonesia.
Professor Faiz Shah
Professor Faiz is a public health physician, development professional, and social entrepreneur with four decades leading innovative initiatives and building grassroots capacity for transformational change. Since his permanent faculty position in community medicine at AI Medical College in 1986, he has taught at leading institutions in the US and Asia. He directs the Yunus Center at Asian Institute of Technology, co-leading the Yunus Masters in Social Business & Entrepreneurship and the ESG Masters programs. He is founding president of Yunus Thailand, and managing partner, Grameen Options. As research partner for the Portable Health Clinic since 2011, he has led pilots in Pakistan and Thailand and contributed to a number of publications.
Dr. Naoki Nakashima
Professor Dr. Nakashima is the Director/Professor (2014- ) of the Medical Information Center of Kyushu University Hospital, and also Vice CIO of Kyushu University, Japan. He has been a specialist of diabetes mellitus for more than 30 years and simultaneously worked as a specialist of medical informatics for 20 years. He is the president of Japan Association for Medical Informatics (JAMI) from June 2019 for three years. He has also been the president of Asia Pacific Association for Medical Informatics (APAMI) from January 2021. Simultaneously, he became the regional vice president of International Medical Informatics Association (IMIA).
Professor Nakashima focuses on the methodologies of disease management and patient-engagement in chronic diseases from primary to tertiary prevention, including personal health record (PHR), telemedicine, IoT sensor network, cyber physical system, data driven medical study, learning health system, and artificial intelligence.
References
1. Meskó B, Drobni Z, Bényei É, Gergely B, Győrffy Z. Digital health is a cultural transformation of traditional healthcare. Mhealth. 2017;3:38-.
2. Coughlin S, Roberts D, O’Neill K, Brooks P. Look-ing to tomorrow’s healthcare today: a participa-tory health perspective. Internal Medicine Journal. 2018;48(1):92-6.
3. O'Shea CJ, McGavigan AD, Clark RA, Chew DPB, Ganesan A. Mobile health: an emerging technolo-gy with implications for global internal medicine. Intern Med J. 2017;47(6):616-9.
4. Helbostad JL, Vereijken B, Becker C, Todd C, Tar-aldsen K, Pijnappels M, et al. Mobile Health Ap-plications to Promote Active and Healthy Ageing. Sensors. 2017;17(3):622.
5. Kostkova P. Grand Challenges in Digital Health. Frontiers in Public Health. 2015;3(134).
6. Nakashima N, Nohara Y, Ahmed A, Kuroda M, Inoue S, Ghosh PP, Islam R, Hiramatsu T, Koba-yashi K, Inoguchi T and Kitsuregawa M. “An Af-fordable, Usable and Sustainable Preventive Healthcare System for Unreached People in Bang-ladesh”. Studies in Health Technology and Infor-matics , 1051, 2013.01.
7. Nohara Y, Nakashima N, Ahmed A, Kuroda M, Inoue S, Ghosh PP, Islam R, Hiramatsu T, Koba-yashi K, Inoguchi T and Kitsuregawa M. “Portable Health Clinic Packages for BoP”. World Congress on Medical and Health Informatics, 1268 , 2013.08.
8. Ahmed A, Hargrave AR, Nohara Y, Kai E, Ripon ZH and Nakashima N. “Targeting Morbidity in Unreached Communities Using Portable Health Clin-ic System”. IEICE Trans Commun , 10.1587/transcom.E97.13.540, E97-B, (3):540-545, 2014.03.
9. Baba Y, Kashima H, Nohara Y, Kai E, Ghosh PP, Islam R, Ahmed A, Kuroda M, Inoue S, Hiramatsu T, Kimura M, Shimizu S, Kobayashi K, Tsuda K, Sugiyama M, Blondel M, Ueda N, Kitsuregawa M and Nakashima N. “Predictive Approaches for Low-Cost Preventive Medicine Program in Devel-oping Countries”. KDD'15, 10.1145/2783258.2788587, 1681-1690, 2015.08.
10. Yokota F, Ahmed A, Islam R, Nishikitani M, Kiku-chi K, Nohara Y, Okajima H, Kitaoka H and Nakashima N. “The relationship and risk factors associated with hypertension, diabetes, and pro-teinuria among adults from Bheramara Upazila, Bangladesh: Findings from Portable Health Clinic Data, 2013-2016”. International Journal of Medi-cal Research and Health Sciences. 7 (2): 1-12. 2018.
11. Hoque R, Sorwar G, Ahmed A and Islam R. “De-velopment of Mobile Based In-Home Patient Mon-itoring System for the Management of Chronic Disease of Indigenous Communities in a Develop-ing Country”. Springer, Cham, 2019. https://doi.org/10.1007/978-3-030-21935-2_27
12. Islam R, Nohara Y, Rahman MJ, Sultana N, Ahmed A and Nakashima N. “Portable Health Clinic: An Advanced Tele-Healthcare System for Unreached Communities”, Ebook: MEDINFO 2019: Health & Wellbeing e-Network for All, Volume 264, 416-419, 2019.08.
13. Islam R, Rahman MJ, Ahmed A and Nakashima N. "GramHealth: Tele-Pathology System for PHC Telemedicine Service". The 4th Digital Pathology CONGRESS: ASIA, Tokyo, 2018.05.
14. Kikuchi K, Sato Y, Izukura R, Nishikitani M, Kato K, Morokuma S, Nessa M, Nohara Y, Yokota F, Ahmed A, Maruf RI and Nakashima N. “Portable health clinic for sustainable care of mothers and newborns in rural Bangladesh”. Journal of Com-puter Methods and Programs in Biomedicine, 207 (2021). Doi:10.1016/j.cmpb.2021.106156
15. Islam R, Yokota F, Nishikitani M, Kikuchi K, Sato Y, Izukura R, Rahman MM, Chowdhury MR, Ah-med A and Nakashima N. “Portable health clinic COVID-19 system for remote patient follow-up ensuring clinical safety”. Journal of Computer Methods and Programs in Biomedicine Update, 2 (2022). Doi: 10.1016/j.cmpbup.2022.100061
16. Pang N, Lasimbang HB, Hijazi MHA, Hamild MNB, Dris MAB, Shoesmith W, Yokota F, Maruf RI and Nakashima N. “OHIDAS Toolkit, the PHC, and Tanya Pakar: A Multi-level, Vertically Integrated Digital Health Promotion, Primary Prevention and Telemedicine Provision Programme”. The Int’l Conference of the Asia-Pacific Association for Medical Informatics (APAMI2020) Proceedings, 120-124, Hamamatsu, Japan, 2020.11.
17. Furukawa Y, Yokota F, Islam R, Nishikitani M, Kikuchi K, Ahmed A and Nakashima N. “School-based educational intervention to improve chil-dren’s oral health-related behaviors in rural Bang-ladesh”. South East Asia Journal of Public Health, http://dx.doi.org/10.3329/seajph.v7i2.38853, 7(2):27-33, 2018.11.
18. Hu M, Sugimoto M, Hargrave AR, Nohara Y, Moriyama M, Ahmed A, Shimizu S and Nakashima N. “Health Checkup and Telemedicine System in Post-Disaster Situations”. Japanese Journal of Telemedicine and Telecare, 11(2):135-138, 2015.05.
19. Khan TR, Hossein KM, Islam R, Fukuda A and Ahmed A. “Measurement of Illness and Wellness Score of Non-Communicable Disease Patients”. The IEEE TENCON. Penang, Malaysia, 2017.11.
20. Islam R, Yokota F, Kikuchi K, Nishikitani M, Izu-kura R, Sato Y, Rahman M, Sultana N, Nessa M, Ahmed A and Nakashima N. “Standardization of Personal Health Records in the Portable Health Clinic System”, IMIA MedInfo 2021, Australia, Oct 2-4, 2021.
Address for Correspondence
Rafiqul Islam (Maruf), PhD
Medical Information Center, Kyushu University Hospital
3-1-1, Maidashi, Higashi-Ku, Fukuoka 812-8582, Japan.
Email: islam.rafiqul.072@m.kyushu-u.ac.jp
Phone: +81 92-642-6994/5881
2. Coughlin S, Roberts D, O’Neill K, Brooks P. Look-ing to tomorrow’s healthcare today: a participa-tory health perspective. Internal Medicine Journal. 2018;48(1):92-6.
3. O'Shea CJ, McGavigan AD, Clark RA, Chew DPB, Ganesan A. Mobile health: an emerging technolo-gy with implications for global internal medicine. Intern Med J. 2017;47(6):616-9.
4. Helbostad JL, Vereijken B, Becker C, Todd C, Tar-aldsen K, Pijnappels M, et al. Mobile Health Ap-plications to Promote Active and Healthy Ageing. Sensors. 2017;17(3):622.
5. Kostkova P. Grand Challenges in Digital Health. Frontiers in Public Health. 2015;3(134).
6. Nakashima N, Nohara Y, Ahmed A, Kuroda M, Inoue S, Ghosh PP, Islam R, Hiramatsu T, Koba-yashi K, Inoguchi T and Kitsuregawa M. “An Af-fordable, Usable and Sustainable Preventive Healthcare System for Unreached People in Bang-ladesh”. Studies in Health Technology and Infor-matics , 1051, 2013.01.
7. Nohara Y, Nakashima N, Ahmed A, Kuroda M, Inoue S, Ghosh PP, Islam R, Hiramatsu T, Koba-yashi K, Inoguchi T and Kitsuregawa M. “Portable Health Clinic Packages for BoP”. World Congress on Medical and Health Informatics, 1268 , 2013.08.
8. Ahmed A, Hargrave AR, Nohara Y, Kai E, Ripon ZH and Nakashima N. “Targeting Morbidity in Unreached Communities Using Portable Health Clin-ic System”. IEICE Trans Commun , 10.1587/transcom.E97.13.540, E97-B, (3):540-545, 2014.03.
9. Baba Y, Kashima H, Nohara Y, Kai E, Ghosh PP, Islam R, Ahmed A, Kuroda M, Inoue S, Hiramatsu T, Kimura M, Shimizu S, Kobayashi K, Tsuda K, Sugiyama M, Blondel M, Ueda N, Kitsuregawa M and Nakashima N. “Predictive Approaches for Low-Cost Preventive Medicine Program in Devel-oping Countries”. KDD'15, 10.1145/2783258.2788587, 1681-1690, 2015.08.
10. Yokota F, Ahmed A, Islam R, Nishikitani M, Kiku-chi K, Nohara Y, Okajima H, Kitaoka H and Nakashima N. “The relationship and risk factors associated with hypertension, diabetes, and pro-teinuria among adults from Bheramara Upazila, Bangladesh: Findings from Portable Health Clinic Data, 2013-2016”. International Journal of Medi-cal Research and Health Sciences. 7 (2): 1-12. 2018.
11. Hoque R, Sorwar G, Ahmed A and Islam R. “De-velopment of Mobile Based In-Home Patient Mon-itoring System for the Management of Chronic Disease of Indigenous Communities in a Develop-ing Country”. Springer, Cham, 2019. https://doi.org/10.1007/978-3-030-21935-2_27
12. Islam R, Nohara Y, Rahman MJ, Sultana N, Ahmed A and Nakashima N. “Portable Health Clinic: An Advanced Tele-Healthcare System for Unreached Communities”, Ebook: MEDINFO 2019: Health & Wellbeing e-Network for All, Volume 264, 416-419, 2019.08.
13. Islam R, Rahman MJ, Ahmed A and Nakashima N. "GramHealth: Tele-Pathology System for PHC Telemedicine Service". The 4th Digital Pathology CONGRESS: ASIA, Tokyo, 2018.05.
14. Kikuchi K, Sato Y, Izukura R, Nishikitani M, Kato K, Morokuma S, Nessa M, Nohara Y, Yokota F, Ahmed A, Maruf RI and Nakashima N. “Portable health clinic for sustainable care of mothers and newborns in rural Bangladesh”. Journal of Com-puter Methods and Programs in Biomedicine, 207 (2021). Doi:10.1016/j.cmpb.2021.106156
15. Islam R, Yokota F, Nishikitani M, Kikuchi K, Sato Y, Izukura R, Rahman MM, Chowdhury MR, Ah-med A and Nakashima N. “Portable health clinic COVID-19 system for remote patient follow-up ensuring clinical safety”. Journal of Computer Methods and Programs in Biomedicine Update, 2 (2022). Doi: 10.1016/j.cmpbup.2022.100061
16. Pang N, Lasimbang HB, Hijazi MHA, Hamild MNB, Dris MAB, Shoesmith W, Yokota F, Maruf RI and Nakashima N. “OHIDAS Toolkit, the PHC, and Tanya Pakar: A Multi-level, Vertically Integrated Digital Health Promotion, Primary Prevention and Telemedicine Provision Programme”. The Int’l Conference of the Asia-Pacific Association for Medical Informatics (APAMI2020) Proceedings, 120-124, Hamamatsu, Japan, 2020.11.
17. Furukawa Y, Yokota F, Islam R, Nishikitani M, Kikuchi K, Ahmed A and Nakashima N. “School-based educational intervention to improve chil-dren’s oral health-related behaviors in rural Bang-ladesh”. South East Asia Journal of Public Health, http://dx.doi.org/10.3329/seajph.v7i2.38853, 7(2):27-33, 2018.11.
18. Hu M, Sugimoto M, Hargrave AR, Nohara Y, Moriyama M, Ahmed A, Shimizu S and Nakashima N. “Health Checkup and Telemedicine System in Post-Disaster Situations”. Japanese Journal of Telemedicine and Telecare, 11(2):135-138, 2015.05.
19. Khan TR, Hossein KM, Islam R, Fukuda A and Ahmed A. “Measurement of Illness and Wellness Score of Non-Communicable Disease Patients”. The IEEE TENCON. Penang, Malaysia, 2017.11.
20. Islam R, Yokota F, Kikuchi K, Nishikitani M, Izu-kura R, Sato Y, Rahman M, Sultana N, Nessa M, Ahmed A and Nakashima N. “Standardization of Personal Health Records in the Portable Health Clinic System”, IMIA MedInfo 2021, Australia, Oct 2-4, 2021.
Medical Information Center, Kyushu University Hospital
3-1-1, Maidashi, Higashi-Ku, Fukuoka 812-8582, Japan.
Email: islam.rafiqul.072@m.kyushu-u.ac.jp
Phone: +81 92-642-6994/5881